- HUMAN Diagnostics Worldwide
- Lab Professionals
- Trends & Topics
Senegal on the right track to eliminate Malaria

LAMP Molecular Diagnostics implementation strategy in Senegal
Malaria is endemic throughout Senegal and 100 percent of the population is at risk of the disease.
The number of malaria cases declined by 38% from 2015–2019 (from 69 per 1000 population to 50) and the number of malaria deaths decreased by 7.1% in the same period (from 0.30 per 1000 population to 0.28)1. This has been achieved by adopting several strategies including diagnosis through rapid tests and a package of population-wide test and treating protocols2.
Following this success, the National Malaria Control Program (Programme National de Lutte contre le Paludisme- PNLP) shifted its strategy from control to elimination and partnered with stakeholders to conduct implementation research on potential elimination strategies in different transmission settings to inform the national malaria strategic plan.
In April 2021, a novel molecular diagnostic tool (LAMP) has been implemented as an additional effort to reach The Senegal 2021–2025 National Strategic Plan (NSP) for the elimination of Malaria.
Malaria epidemiological situation in Senegal
The burden of malaria in Senegal is still unevenly distributed with a lower rate transmission in the northern part of the country. Three regions, Kolda, Tambacounda and Kédougou, carry the bulk of the burden.
- 11% general population
- 83% of confirmed malaria cases of all ages
- 90% of cases in children under 5 years of age
- 90% of cases in pregnant women.
- 51% of deaths of all ages
- 73% of deaths in children under 5 years old
The proportional malaria morbidity has decreased from 1.90% in 2015 to 1.09% in 2020, a reduction of 42.4%. Proportional malaria mortality decreased from 1.90% in 2015 to 1.01% in 2020, a reduction of 46.7%3.
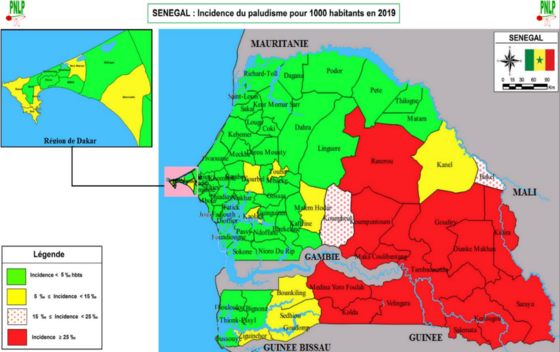
Incidence of Malaria per 1000 population at risk in 2019 (source PNLP)
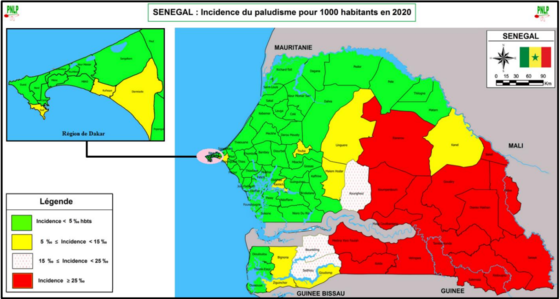
Incidence of Malaria per 1000 population at risk in 2020 (source PNLP)
Malaria-LAMP how does it work
The loop-mediated isothermal amplification (LAMP) is a recently developed molecular technique that was designed to overcome challenges perceived with existing diagnosis tools by being a simpler and faster method than microscopy while still providing a high level of accuracy compared to rapid tests.
1–2 parasites/µL is the limit of detection, which is far lower than microscopy and RDTs. In addition, Malaria-LAMP can differentiate between Plasmodium pan species, P. falciparum and P. vivax, and has a sensitivity of 84–94%, a specificity of >92%4.
The assay has the potential as a reference standard in resource-limited settings; and as a tool for surveillance and screening when a highly sensitive assay is needed. The workflow can be done in a few steps and allows an easy DNA extraction and preparation of reaction mixes, all in one instrument without the need for any additional equipment.
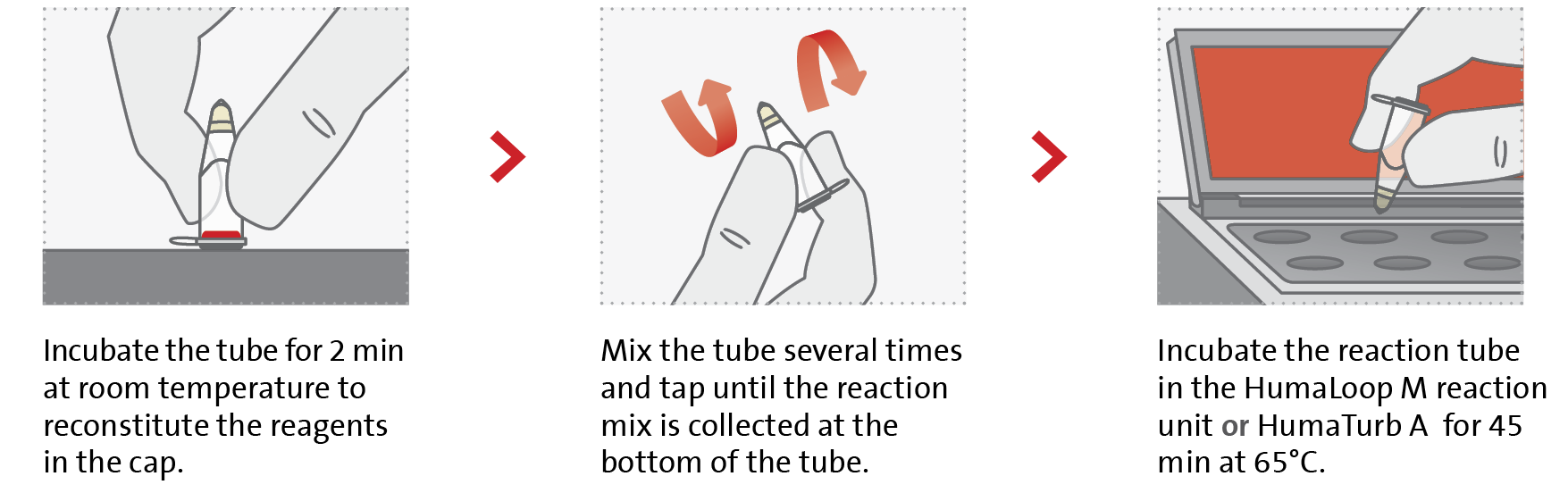
Compared to PCR, Malaria-LAMP has a shorter time-to-result (45 min), a lower cost and the results are visible to the naked eye under blue LED light. Reagent storage and shipment are at room temperature suitable for rural areas with limited settings.
Pilot project for Malaria-LAMP implementation

A 3-years pilot project has been initiated in the fall of 2021 to reduce the gap of detection accuracy of malaria cases in the sites with a lower prevalence.
Financed by the Islamic bank and with technical support and guidance from Human Diagnostics Germany, 30 units of HumaLoop M were purchased, as well as the various detection kits, to be able to carry out a total of 58,000 tests within the first year.
“Train the trainers” program
A designated number of laboratories personnel have received a customized “train the trainers” program that will allow them to carry out the trainings for the rest of personnel in the district laboratories where Humaloop M has been implemented.
Project schedule
The project is scheduled to run for 3 years. A final evaluation will be conducted by the end of the trial period.
As a next phase, more HumaLoop M instruments will be installed in additional sites around Senegal.
A refreshing training has been conducted by the PLNP managers to raise awareness about the LAMP technology and the instructions of use.
Pictures: Dakar Senegal April 2021 - Official Launch of the pilot project Malaria-LAMP
PNLP Guidelines and goals for 2021 -2025
The Senegal is updating their national policies and guidelines in line with the goal of malaria elimination by 2025.
Strengthening the decentralization process through the establishment of regional malaria control plans is one of the main strategic approaches that the government has adopted.
The Use of molecular biology in low prevalence areas for diagnosis, Intensification of cross-border control and the Improvement of projects will accelerate the fight against malaria in the southern and eastern zones of the country.
In June 2021 the PNLP released an updated national guideline for the use of molecular diagnosis LAMP (Loop-Mediated isothermal Amplification) in district-level hospitals.
The use of the "LAMP" technique is indicated in the following situations:
- For quality control of microscopy and RDTs: given the sensitivity providers may request the use of this tool to assess the quality of smear microscopic results and rapid diagnostics test results.
- During case investigations, based on the confirmatory approach before the Focal Screening Test and Treat (FSTAT) or the Focal Test and Treat (FTAT) is a drug administration tool commonly referred to as the Risk Factor Test.
- In case of discrepancy between the RDT and the microscopy in the biological diagnosis of the cases in routine, the tool "LAMP" is indicated to have a result of best quality.
- In case of strong suspicion of malaria with a negative RDT or microscopy result (routine).
References
1. Severe Malaria observatory extension of Medicines of Malaria ventures.
2. Sophie Faye, corresponding author 1 Altea Cico, 1 Alioune Badara Gueye, 2 Elaine Baruwa, 1 Benjamin Johns, 1 Médoune Ndiop, 2 and Martin Alilio 3 Scaling up malaria intervention “packages” in Senegal: using cost effectiveness data for improving allocative efficiency and programmatic decision-making Malar J. 2018; 17: 159.
3. PNLP (Programme National de Lutte contre le Paludisme- PNLP).
4. Mohon AN, Getie S, Jahan N, et al. Ultrasensitive loop mediated isothermal amplification (US-LAMP) to detect malaria for elimination. Malar J. 2019;18(1):350.





